TRICARE provides prescription drug coverage with most TRICARE health plans. If you use the US Family Health Plan, you have a separate pharmacy coverage.
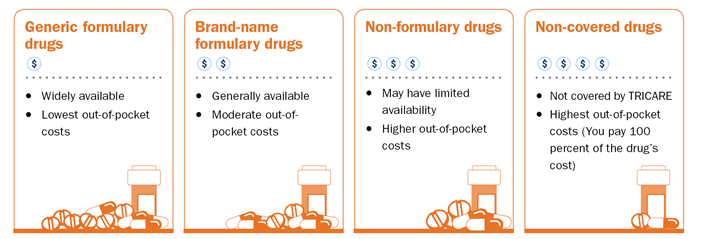
The TRICARE Formulary is a list of generic and brand-name prescription drugs that we cover. TRICARE covers most prescription drugs approved by the Food and Drug Administration (FDA). Prescription drugs may be covered under the pharmacy benefit or the medical benefit. We review and update the TRICARE Formulary each quarter. After each review, some drugs may move from one category to another. You’ll get a letter from Express Scripts if you have a prescription for a formulary drug that’s changing to a non-formulary drug.
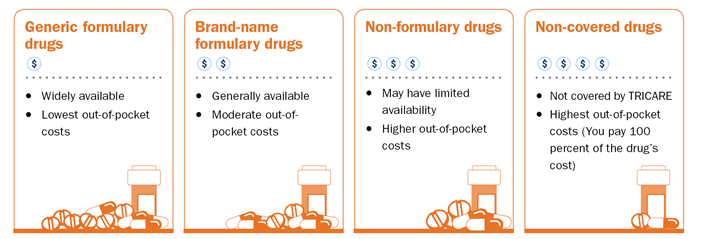
These categories follow industry standards. They depend on the medical effectiveness and cost effectiveness of a drug compared to other similar drugs.
Certain prescriptions require a pre-authorization. You may need pre-authorization for your prescription if it:
Check the TRICARE Formulary to see if you need pre-authorization.
There are specific rules for filling prescriptions for certain types of drugs. Learn more about filling prescriptions for these drugs:
Managing your prescriptions can be tricky, but the TRICARE Formulary Search Tool can help! Learn how much you’ll pay, where you can get your prescriptions filled, and so much more.
Starting March 1, 2024, you may start to receive expanded specialty pharmacy services from Accredo. Accredo is an accredited specialty pharmacy that serves patients with complex and chronic health conditions. >>Learn more
Quantity limits vary by type of pharmacy:
Exceptions can be made if your provider establishes medical necessity.